Editor-in-Chief
- FMA
- The Fabricator
- FABTECH
- Canadian Metalworking
Our Publications
Categories
- Additive Manufacturing
- Aluminum Welding
- Arc Welding
- Assembly and Joining
- Automation and Robotics
- Bending and Forming
- Consumables
- Cutting and Weld Prep
- Electric Vehicles
- En Español
- Finishing
- Hydroforming
- Laser Cutting
- Laser Welding
- Machining
- Manufacturing Software
- Materials Handling
- Metals/Materials
- Oxyfuel Cutting
- Plasma Cutting
- Power Tools
- Punching and Other Holemaking
- Roll Forming
- Safety
- Sawing
- Shearing
- Shop Management
- Testing and Measuring
- Tube and Pipe Fabrication
- Tube and Pipe Production
- Waterjet Cutting
Industry Directory
Webcasts
Podcasts
FAB 40
Advertise
Subscribe
Account Login
Search
How 3D knee replacement and robots can improve surgery
Stryker uses additive manufacturing and robotics to promote bone/implant bonding and shorten post-surgery recovery times
- By Don Nelson
- Updated January 24, 2023
- April 26, 2021
- Article
- Additive Manufacturing

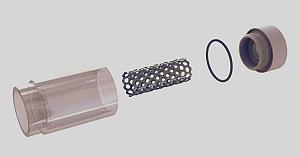
Stryker’s Triathlon implant has four components (from top): femur, patella (attached to the femur), liner, and tibia. Images: Stryker
Total knee replacement surgery has intrigued me since 1979, when my grandfather had the procedure performed on both knees. The prostheses of that era were designed to anatomically mimic the motion of a knee joint, making them superior to their hinge-action predecessors of the ’60s.
But as I’ve discovered since undergoing my own knee replacement surgery last November, today’s prostheses, surgical techniques, and patient outcomes have vastly improved since Gramps was rolled into the operating room. Advancements in what’s medically known as total knee arthroplasty (TKA) include materials developed specifically for implants and their 3D-printed components, as well as the use of surgical-assist robots.
To learn more about TKA and 3D printing’s role in producing implants, I contacted Stryker Corp., the manufacturer of my new knee and the robot that assisted with its implantation.
I spoke with Robert Cohen, president of Stryker’s Digital, Robotics, and Enabling Technologies entity. Cohen, who earned multiple engineering degrees at New Jersey Institute of Technology in the 1980s, has spent his career manufacturing implants. He also has unfettered enthusiasm for how digital technologies like 3D printing help engineers improve TKA surgery, with “help” being the operative word.
He describes additive manufacturing as a “tool” that aids engineers in discovering solutions to problems that can’t be solved by conventional manufacturing methods. “3D printing by itself is nothing but fancy printing—another way to manufacture.”
What drives innovation are the “skillsets of people who want to solve problems in new ways and come up with, in our case, new implants. 3D printing is the enabler that [makes their] designs reality,” he said.
Stryker began adopting additive manufacturing technologies in 2002. Besides knees, the global corporation headquartered in Kalamazoo, Mich., also 3D-prints hips, spinal cages, and other implantable devices. AM allows the company to produce prosthetic geometries that would be impossible or impractical to manufacture by traditional methods. An example is additively manufactured scaffolds that promote biologic fixation—the growth of bone into a prosthetic.
“3D printing is the only way to do that,” said Cohen. “Bone wants to grow into something. Instead of just doing a line-of-sight process, where you might drill holes, and say, ‘Hey, bone, I hope you grow into the holes.’ Now we can print a scaffold structure and bone will grow into it, and the scaffold has structural integrity at the same time. Just like a railroad trestle.”
Growth of TKAs
I wasn’t the only passenger who boarded the TKA train last year. It’s estimated that more than 600,000 Americans annually receive the surgery—a figure expected to rise in the coming decade. The combined number of hip and knee replacement procedures in the U.S. is about 1 million yearly.
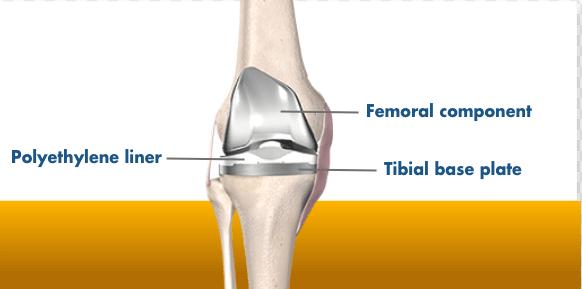
My surgical team at NorthShore Medical Group-Skokie, outside Chicago, used Stryker’s Triathlon total knee system and was assisted by the medical device manufacturer’s Mako surgical robot. The cementless implant incorporates a femur, tibia, patella, and polyethylene liner.
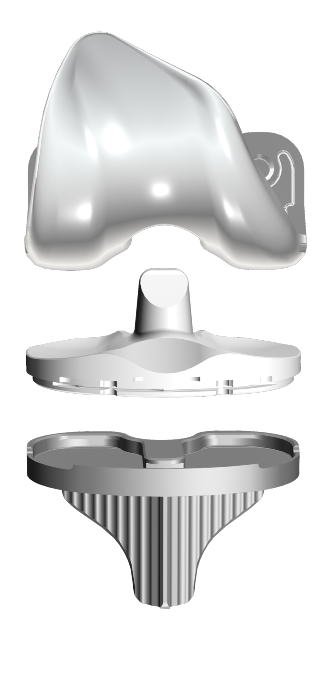
The Triathlon’s additive components are made from a titanium alloy Stryker developed for 3D printing.
The use of cementless knees has grown rapidly the past few years. The reason is because bone cement, long used for TKA surgeries, is an interface that can break down, said Cohen. “It’s another opportunity for the implant to loosen.”
Stryker casts the femoral component of a Triathlon knee from cobalt chromium, a material that interacts well with the plastic liner. After casting, the femur is finish-machined and coated with sintering beads that promote bone ingrowth.
During TKA surgery, a series of box cuts are made on the patient’s femur. The two cuts on the end interface with the implant like a wedge being pounded into a piece of wood. “That’s the most stable surface ever,” said Cohen. “Think about it. You’re standing up, so you’re always sort of pushing the [bone] tighter into place.”
Producing the patella is a comparatively straightforward process. The metal-backed patella is fitted with a 3D-printed geometry made from Tritanium, a titanium alloy Stryker developed specifically for AM applications in which bone ingrowth is desirable.
Tritanium also is used to 3D-print the tibial baseplate. It forms a virtually fail-proof bond with the patient’s tibia using an interference-fit connection, a force that relies on friction to hold together two mating, tightly fitting objects. The main features of the metal baseplate’s design are four pegs and a keel.
Cohen said, “With additive manufacturing, we can put those posts and keel where they’ll all work together to create an interference fit.” It is “rock solid.” He added that machining the baseplate couldn’t be justified economically. “The cost would be outlandish.”
Manufacturing Overview of 3D Knee Replacement
For AM applications, Stryker mostly uses direct metal laser sintering (DMLS) printers. “We were doing some electron-beam processes for larger metal parts,” said Cohen, “and we’re looking at different printers for [complex] jigs and fixtures and for disposable instruments and polymers. There are some polymers that could be used for an implant, and there are some polymers that could be single-use surgical instruments, depending on the material requirements.”
Selecting and bringing a 3D printer online to build prostheses is a major undertaking. In the world of metal load-bearing implants, it would be unrealistic to buy a DMLS printer, plug it in, and expect to make an implant.
Printing metal implants requires learning to control the laser, melt pool, wattage and feeds, layering, and many other process parameters. “Because we’ve built competencies in those areas,” said Cohen, “we’re one of the few companies in health care, in the world, that has the capability to scale up and not just do small-run production.”
The corporation’s scaling capabilities have been augmented by its AMagine Institute, a global technology development center located in Cork, Ireland. Reportedly the world’s largest facility dedicated to additively manufacturing orthopedic components, Cohen said the institute’s production personnel 3D-print more than 1 million parts annually.
3D Knee Replacement Robot-Assisted Surgeries
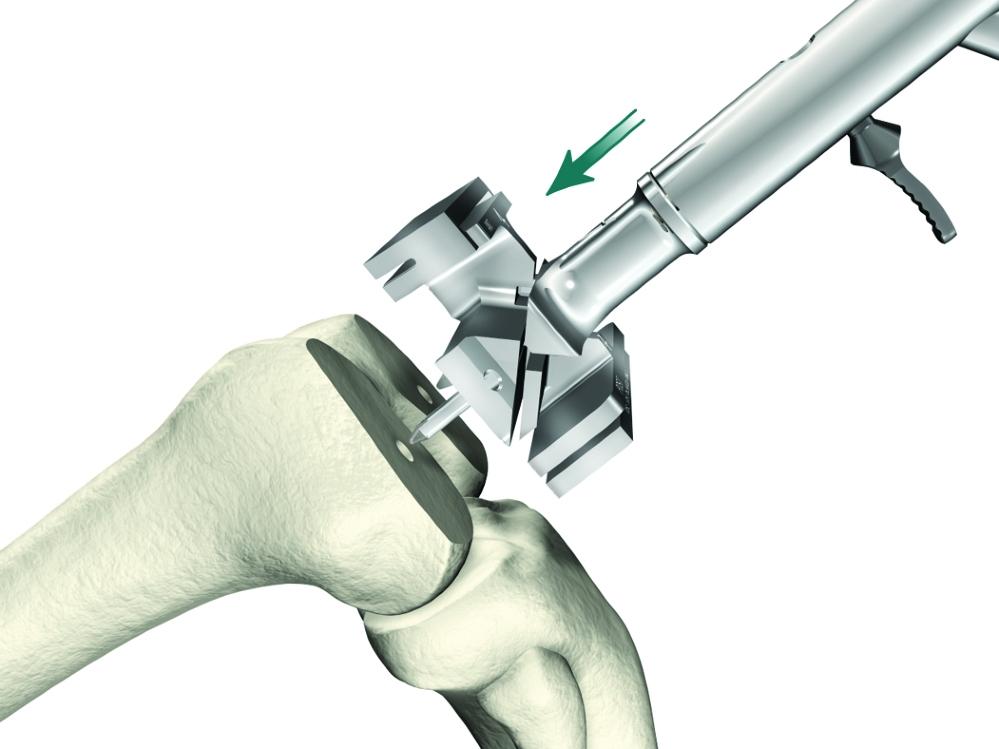
A much smaller though equally impressive sum is 1,000—the number of Mako robot-assist systems Stryker has placed in hospitals the past three years. A Mako robot, which costs more than $1 million, according to published reports, is used to implant Triathlon knees. The system determines final bone preparation and implantation steps to be executed with special Triathlon instruments.
Cohen said 42% of the primary knees that Stryker sells in the United States are implanted with a Mako robot. He expects the percentage to rise to 50% soon.
As is the case with learning to 3D-print TKA components, developing a surgical robot isn’t a task for the impatient or inexperienced. Cohen said, “We design the robots. We write the software, and we build the robots ourselves because nobody else can do it. We have worked on this for over a decade.”
A key benefit of the robotic system is that it provides the surgical team unprecedented amounts of data about the patient’s knee before and during surgery. The process starts with the hospital taking a CT scan of a patient’s knee prior to admittance. The hospital sends the scan to Stryker, which creates a virtual 3D model of the knee joint, tibia, femur, patella, cartilage, and ligaments. The scan also reveals useful information like the amount of arthritic damage the patient has incurred and joint-space narrowing caused by cartilage loss.
The next step is to match the data with a virtual implant. Stryker team members position virtual models of the femur and tibia on the virtual bones and gather data on rotation, X-Y-Z axes, tilt, slant—“everything you could possibly need to match you is individualized,” Cohen explained. The team also re-establishes the patient’s joint line, in three dimensions.
“The purpose of the robot is to get your knee exactly on your joint line … and to make surfaces that last your lifetime,” said Cohen.
Once all the data is gathered, Stryker bundles it into a plan for the surgery that is sent to the surgeon. The plan is loaded into the robot before the patient enters the operating room. But it’s not the final surgical plan, Cohen pointed out. While the patient is under anesthesia, the surgeon bends the TKA knee and the robot tracks the bending action.
“So let’s say your ligaments are a little bit too loose, and the surgeon running the robot looks at the screen and says, ‘Ah, you know, the medial [collateral ligament] is a little bit lax. So we’re going to move the tibial component up a little bit, twist the femur, and now let’s flex the knee again—virtually—and see what the end surgery would look like in terms of flexion.’ ”
Once the plan has been fine-tuned and completely individualized, it’s locked in and surgery commences.
During the operation, the robot controls the motion of surgical instruments. For example, as the surgeon pushes a saw into a bone, the robot controls the plane of the blade and executes the cut with an accuracy and precision unseen in surgery before, said Cohen.

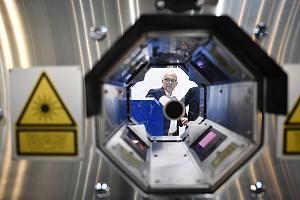
Robert Cohen, president of Stryker’s Digital, Robotics, and Enabling Technologies entity, has spent his entire career manufacturing prostheses.
The forward progress of the blade is controlled too. This prevents it from entering healthy tissue once the bone has been cut clean through. “We have haptics built into the robot arm,” said Cohen. “The saw stops automatically when you hit the bone’s boundary. We create a bubble, a safety zone.”
Better Outcomes for Knee Replacements
From the patient’s perspective, the biggest benefit of robot-assisted surgery is a shorter recovery time. This is largely a result of minimizing damage to healthy tissue and proper placement of the prosthetic.
Cohen said, “When you wake up [after surgery], you’re flexing in the right spot. You don’t have to relearn to walk, like in 1979 when implants were put in the wrong spot. Now you have less physical therapy sessions. You return to flexion earlier. You get relief from pain sooner because you didn’t have as much soft-tissue trauma. You can go back to work sooner. You don’t have any of the health issues.
“There are fewer re-admissions and re-operations. You have higher patient satisfaction.”
Personal Outcome
TKA surgery is major surgery. More “majorly” than I imagined before entering the hospital last November. (A bit of unsolicited advice: If you’re contemplating knee surgery, don’t watch a YouTube video of the procedure before the operation. Wait until after.) My biggest takeaway from the experience is that the return to mobility was much faster than expected.
My grandfather was bed-ridden for more than a week after his TKA surgeries. He spent weeks in rehabilitation before he was able to walk—with the aid of a walker. And although the implants greatly enriched his life, he needed two canes to get around for the rest of his days.
The circumstances surrounding my TKA surgery were different than my grandfather’s. I was nearly 20 years younger, and I only had one knee operated on. I also was a “good” candidate for the surgery in that I was fit and had regularly done exercises to strengthen the muscles supporting the knee for the 15 years preceding the operation.
Still, eight hours after the procedure, I easily circumnavigated the orthopedic floor of the hospital with the assistance of a walker. I was discharged from the hospital 24 hours after surgery. And two days after the operation, on Thanksgiving Day, I was able to walk a half mile unaided.
It was a satisfying walk.
SIDEBAR
Knee implant surgery runs in the family

The Mako surgical robot helps prevent damage to healthy tissue and locates the knee implant correctly on the patient’s bones.
I’m not the first member of my family to take a prosthetic knee.
My grandfather had both knees replaced in 1979, at the age of 85. He became one of the earliest adopters of the then-rare procedure so he could continue to tend his garden. My mother-in-law had her knees replaced about 20 years ago, at 65, out of a desire to play tennis and tend to her grandchildren.
The reasons people choose to have total knee replacements today are different than they were 40 years ago. Robert Cohen, president of Stryker’s digital manufacturing entity, said the most common reason is to enhance mobility.
“Thirty years ago, a person 75 years old may have just wanted an implant to relieve pain,” he said. “Now, somebody 75, 80 years old wants to be able to walk a golf course ... sit on the floor with a grandkid and get up off the floor unaided.”
This desire has boosted the number of knee surgeries performed and attracted younger adults who want the procedure. Stryker has manufactured knees for individuals in their 40s, 30s, and even 20s, said Cohen. “We had someone who has a partial knee who rides in the Tour de France.”
No member of my family has qualified to compete for the yellow jersey, but those of us who have had the surgery were glad we did. My grandfather worked in his garden until he died, at 96, and my mother-in-law still plays tennis and keeps up as best she can with her now-adult grandchildren.
My main reason for having the procedure was to continue my regimen of walking three to five miles a day without pain. Five months after surgery, I’m back to walking three miles daily pain-free. –D. Nelson
About the Author
Don Nelson
2135 Point Blvd.
Elgin, IL 60123
(815)-227-8248
About the Publication
- Podcasting
- Podcast:
- The Fabricator Podcast
- Published:
- 04/16/2024
- Running Time:
- 63:29
In this episode of The Fabricator Podcast, Caleb Chamberlain, co-founder and CEO of OSH Cut, discusses his company’s...
- Trending Articles
- Industry Events
16th Annual Safety Conference
- April 30 - May 1, 2024
- Elgin,
Pipe and Tube Conference
- May 21 - 22, 2024
- Omaha, NE
World-Class Roll Forming Workshop
- June 5 - 6, 2024
- Louisville, KY
Advanced Laser Application Workshop
- June 25 - 27, 2024
- Novi, MI